Are you between 8-13 years old? Have you recently increased your activity levels or returned to football? Do you have sore heels that are worst when wearing football boots or going barefoot? If so, you may be suffering from Sever's Disease. Contrary to its name, Sever's Disease is not actually a disease. It is a common heel condition that affects children within a specific age range. Let's delve into what Sever's Disease is and how you can manage it.
What is Sever's Disease?
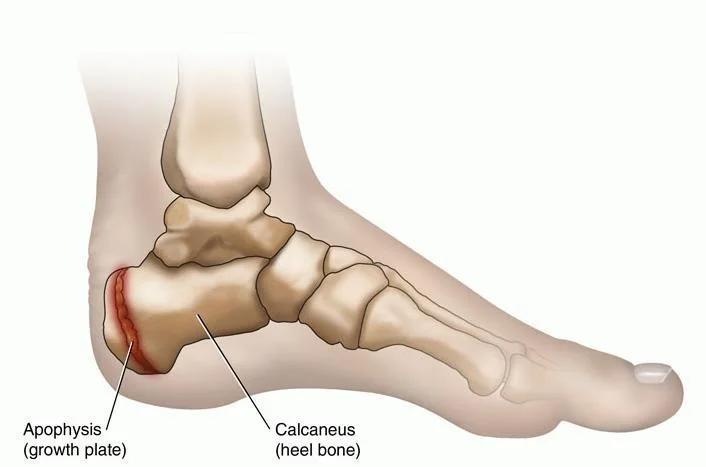
Sever's Disease is a periodic condition that typically presents between the ages of 8-13 years for a duration of 6-12 months. It occurs because the growth plate at the back of the heel bone (calcaneus) is open and more fragile during this stage of development. Increased strain on this area, due to the pull of the Achilles tendon and shock on the heel bone, leads to heightened pain and discomfort.
Symptoms:
If you're experiencing Sever's Disease, you may notice the following symptoms:
Heel pain that worsens with physical activity
Tenderness in the back of the heel
Difficulty walking or running
Treatment Options:
Managing Sever's Disease involves a combination of strategies. Here are some initial treatment options to alleviate symptoms:
Activity reduction: It's important to decrease the intensity and frequency of activities that worsen the heel pain. Give your heels some rest to allow the growth plate to heal.
Orthotics: Custom and orthotic options are available that will manage the condition to varying degrees. An orthotic will assist in cushioning the calcaneus (heel bone) and supportive the foot function that can be contributing to the condition.
Calf stretches: Regular stretching of the calf muscles can help reduce strain on the Achilles tendon, which in turn eases the pressure on the heel bone. Perform gentle calf stretches several times a day.
Heel raises: By wearing shoes with cushioned heels or using heel cups, you can provide additional support and shock absorption to the affected area. This can help reduce pain and discomfort.
Ice application: Applying ice packs to the affected heels for about 15-20 minutes at a time, several times a day, can help alleviate inflammation and provide temporary pain relief.
Supportive footwear: Opt for shoes with good arch support and cushioning to minimize stress on the heel. Avoid flat or unsupportive footwear that can exacerbate symptoms.
Physical therapy: In some cases, a physical therapist may recommend specific exercises to strengthen the foot and ankle muscles, improve flexibility, and correct any biomechanical issues that may contribute to Sever's Disease.
Prevention:
Preventing Sever's Disease or reducing the risk of recurrence is possible. Here are some preventive strategies:
Gradually increase activity levels: Avoid sudden spikes in physical activity. Gradually build up your activity levels to allow your body to adapt.
Warm-up and cool-down routines: Prior to engaging in sports or exercise, perform a proper warm-up routine to prepare your muscles and joints. Similarly, cool down afterward with gentle stretching to aid recovery.
Choose appropriate footwear: Ensure your shoes provide proper arch support, cushioning, and a good fit. Replace worn-out shoes regularly.
Maintain foot and ankle strength: Engage in exercises that strengthen the foot and ankle muscles, such as toe curls, heel raises, and balance exercises.
Listen to your body: Pay attention to any signs of heel pain or discomfort and seek medical advice promptly. Early intervention can prevent the worsening of symptoms.
Conclusion:
Sever's Disease may cause temporary discomfort and heel pain, but with proper management and care, you can reduce its impact on your daily activities. Remember, it's essential to consult a podiatrist for a comprehensive evaluation and personalized treatment plan. By following the recommended strategies, you can ease your symptoms, recover faster, and get back to your favorite activities with reduced pain.
Remember, it's important to consult a healthcare professional for a proper diagnosis and individualized treatment plan. Take care of your feet, and don't let Sever's Disease hold you back from enjoying an active and healthy lifestyle!
Book an appointment online now, or call the clinic on 3269 0114 to solve your heel pain now.