Imagine experiencing the injury firsthand, truly understanding the pain an athlete goes through. Well, that's exactly what happened to me recently. It began as a small niggle on the outside of my right knee, which I ignored for a few runs. Eventually, it escalated to the point where I hobbled home after my regular 12km run, with shooting pain down to my foot. The excruciating pain immediately after stopping running subsided, but I knew something was wrong. It turned out to be Illiotibial Band Friction Syndrome, or ITBFS, a common condition among active individuals. Let's dive into what ITBFS is and how it can be addressed.
What is ITBFS?
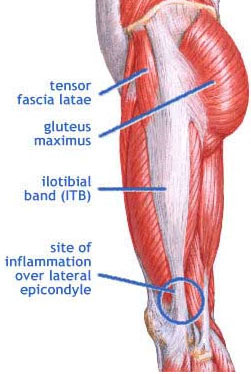
ITBFS is the most frequent cause of lateral knee pain in the active population. It is caused by tightness or friction of the Illiotibial Band (ITB), a long tendon on the outside of the thigh. In many cases, including mine, the ITB exerts increased pressure on the fat pad that allows it to glide smoothly over the lateral knee joint. This heightened pressure can lead to swelling of the fat pad, causing pain. Additionally, it can compress the common peroneal nerve, resulting in shooting pain down to the foot.
What should I do if I have ITBFS?
The ideal course of action is not to ignore the initial "niggle," as I did. As evident in my personal experience, neglecting the pain only leads to increased discomfort and more time away from training. If you notice a niggle, you can try the following:
Ice: Apply ice immediately after exercise to reduce swelling of the fat pad and provide pain relief.
Stretching: Perform ITB stretches to help alleviate tension in the ITB.
Foam Roller: Use a foam roller on the ITB, but avoid rolling directly over the site of pain as it may increase pressure on the fat pad and worsen symptoms.
Exercises: Often, the ITB is overworked due to poor engagement of the hip external rotator muscles, such as the gluteals. Strengthening the gluteal muscles can help ensure they are properly engaged while running.
Training Load: Decrease the specific training load that exacerbates the pain. While complete rest is not usually recommended for ITBFS, finding activities that reduce the load on the ITB, such as swimming or cycling, can be essential for recovery.
What if the pain persists despite these measures?
If you are still experiencing pain, it indicates that there may be additional contributing factors overloading the ITB. This can include inappropriate footwear, poor running mechanics, or muscular strength and flexibility imbalances. At this stage, it is best to consult a trusted sports medicine practitioner. At Principal Podiatry, for example, we conduct biomechanical screenings to assess your running and walking patterns, as well as identify any tightness or other contributing factors.
In my case, a combination of activity modification (swimming), glute strengthening, ITB stretching, and fine-tuning of custom orthotics facilitated a faster recovery. It is important to remember that every individual is unique, and what works for one person may not work for another. That's why professional screenings can determine the most suitable treatment plan tailored specifically to you.
Conclusion:
Illiotibial Band Friction Syndrome (ITBFS) can be a debilitating condition for athletes and active individuals. By understanding its causes and seeking appropriate treatment, you can overcome ITBFS and return to pain-free performance. If you experience any symptoms or discomfort, don't hesitate to consult a sports medicine practitioner or podiatrist who can provide a thorough assessment and personalized treatment plan. With a comprehensive approach addressing contributing factors and utilizing targeted interventions, you can overcome ITBFS and get back to doing what you love.